
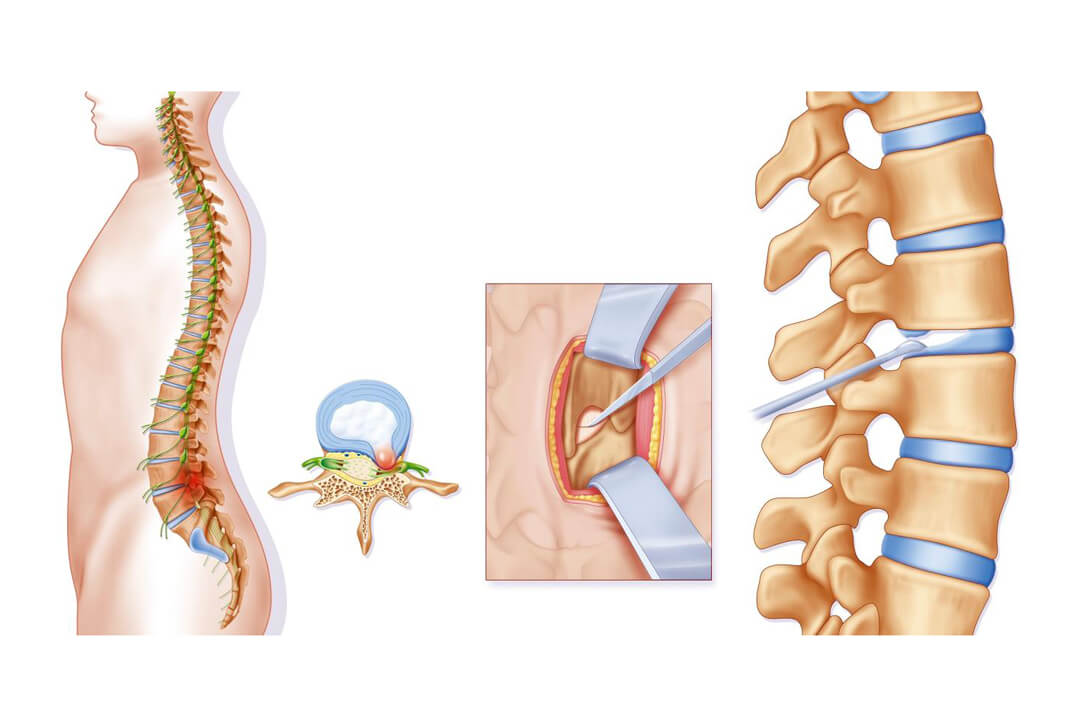
The new endoscopic discectomy technique allows us to treat a herniated disk more safely and in a more tissue-preserving way than ever. The most important difference to a conventional endoscopic procedure is the lateral access through the foramen compared to the traditional dorsal access. By this means, the nerves that run through the spinal canal remain completely untouched and injuries, adhesions and other complications are hence avoided. Also the intervertebral ligaments that stabilize the spinal column stay intact.
As the lateral access allows for a tissue-preserving procedure which is associated with relatively little pain, no general anesthesia is required.
Under local anesthesia an optical endoscope is inserted through a small incision in the skin. It is equipped with tiny working cannulas and is carefully pushed forward to the site of the disk prolapse. The extruded disk tissue can be removed under sight control. Protruding remainders are eliminated by means of a special laser nucleolyser. In certain cases, the gel-like nucleus of the intervertebral disk is shrinked with the aid of chymopapain – a special protein-cleaving enzyme. This helps to disencumber the fibrous ring to support the subsequent healing process. For the revitalization of the spinal disk, abrasion of the calcified vertebral bone by means of minute instruments is done. This leads to a better blood supply in the disk tissue and a firm and stable fibrous ring can develop.
The intervention takes 30 to 45 minutes.
Advantages of endoscopic discectomy at a glance: